Navigating Healthcare Interoperability Standards
HL7 and now FHIR are integral to achieving the dream of connected healthcare, but they are not without their challenges.

In a world choked by data silos, imagine healthcare flowing freely. Where patient records seamlessly transfer between hospitals, doctors, labs, and other health IT solutions, empowering informed decisions and personalized care. This is the dream of healthcare interoperability, and it hinges on the silent heroes called standards. Think of them as translators for the complex languages of healthcare data. Standards like HL7 (Health Level Seven) and FHIR (Fast Healthcare Interoperability Resources) bridge the gaps between disparate systems, ensuring information talks the same language, regardless of origin.
But are these just buzzwords, or do they hold the key to unlocking a new era of coordinated care? In this blog post, we’ll journey through healthcare interoperability standards, demystify the acronyms, and explore the benefits and challenges. We’ll dive into the specifics of HL7 and FHIR, revealing their power to transform healthcare from a fragmented landscape into a united symphony of data.
So, buckle up, fellow data enthusiasts and healthcare heroes, as we explore the transformative potential of healthcare interoperability standards and pave the way for a future where patient information flows like information should – seamlessly, securely, and ultimately, for the benefit of all.
Understanding Healthcare Interoperability Standards
Think of healthcare interoperability standards as the translators of the healthcare world. They bridge the gap between diverse Electronic Health Records (EHRs) by establishing common languages and protocols for data exchange between disparate health IT systems.
There are many benefits to interoperability standards. Streamlining data exchange allows seamless communication between disparate healthcare systems. This results in improved coordination and quality of care. Moreover, adherence to interoperability standards also ensures compliance with regulatory requirements, promoting data security, privacy, and integrity. This is critical for maintaining trust in healthcare information exchange.
Key interoperability standards include:
HL7 (Health Level Seven):
Founded in 1987, Health Level Seven International (HL7) is a globally recognized authority in healthcare information interoperability that develops standards for the seamless exchange of electronic health information. It’s the granddaddy of healthcare data exchange, providing a comprehensive framework for structured clinical data communication. HL7 standards ensure a common language for the exchange of clinical and administrative data between disparate healthcare organizations, regardless of differences in technology or vendor platforms. HL7 has evolved through various versions, each addressing the changing needs of the healthcare industry.
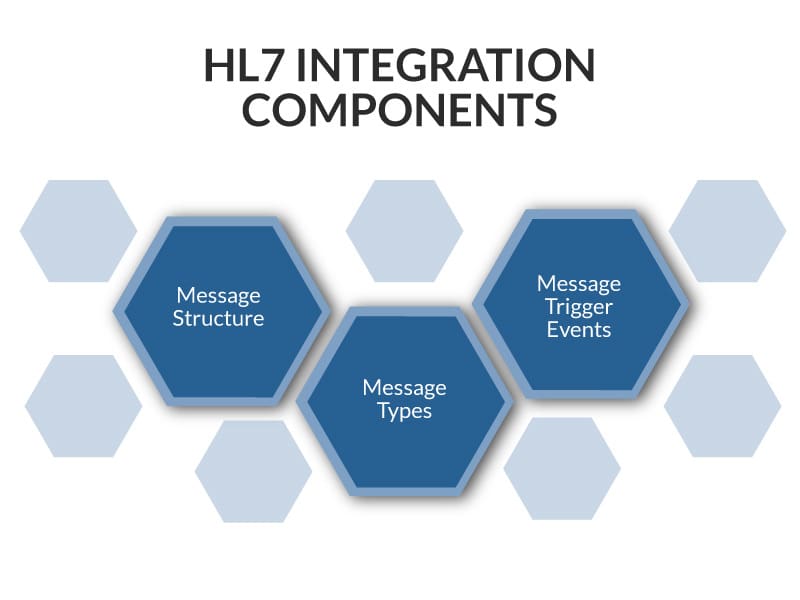
Key components and benefits of HL7:
- Message Structure: HL7 messages are composed of segments, fields, components, and sub-components, with each segment containing distinct categories of data and separated by special characters. Segments are logical groupings of data fields that make up HL7 messages, providing an organized structure for the data within the message.
- Message Types: Several common HL7 message types serve unique purposes in healthcare data exchange, such as ADT (Admit, Discharge, Transfer), ORM (Order message), ORU (observation result), etc. The format of each message type varies, but they all share a common structure. Understanding the different message types and their formats is crucial for accurate healthcare data exchange & integration.
- Message Trigger Events: HL7 trigger events are the catalysts that initiate the exchange of HL7 messages. They are actions or occurrences, such as patient admission (ADT), Order placement (ORM), or lab results reporting (ORU), that prompt the sending of HL7 messages between healthcare systems. These events play a crucial role in ensuring that healthcare data is exchanged accurately and in a timely manner.
Challenges of HL7:
While HL7 standards have significantly contributed to healthcare interoperability, they are not without challenges and limitations. Some of these include:
- Complexity: HL7 standards, particularly HL7 v2, can be complex and challenging to implement. The extensive documentation and varied use cases make it demanding for developers and healthcare organizations to adopt and adhere to the standards.
- Versioning Issues: HL7 has evolved through different versions, and compatibility issues may arise when healthcare systems use different versions. Transitioning from one version to another can be a complex process, potentially causing disruptions in data exchange.
- Variability Interpretation: Despite being a standard, the interpretation and implementation of HL7 standards can vary among healthcare systems and vendors. This variability can lead to challenges in achieving seamless interoperability.
- Limited Support for Modern Technologies: HL7 v2, an older standard, may have limitations in supporting modern technologies and data formats. HL7 FHIR addresses this concern, but transitioning from older versions may still pose challenges.
- Resource Constraints: Implementing HL7 standards may require significant resources in terms of time, expertise, and financial investment. Smaller healthcare organizations with limited resources may find adopting and implementing these standards challenging.
- Semantic Interoperability: While HL7 addresses syntactic interoperability (structuring and formatting data consistently), achieving semantic interoperability (ensuring a common understanding of the meaning of data) remains a challenge. Different interpretations of clinical terms or concepts can hinder true semantic interoperability.
- Resistance to Change: Healthcare systems often have legacy infrastructure and established processes. Implementing HL7 standards may require significant changes to existing workflows and resistance to these changes can impede adoption.
While HL7 falls short of achieving the goal of seamless integration between any health IT system, HL7 did lay the groundwork for better healthcare interoperability. Despite these challenges, ongoing efforts within the HL7 community, including the development of HL7 FHIR, aim to address some of these limitations and provide a more modern and flexible approach to healthcare interoperability.
FHIR (Fast Healthcare Interoperability Resources)
Unlike its complex predecessors, Fast Healthcare Interoperability Resources (FHIR) uses familiar internet technologies like RESTful APIs and JSON to connect diverse systems regardless of their native language. This means no more clunky translations or lost information in the labyrinth of data silos. Introduced by Health Level Seven International (HL7), FHIR represents a modern and web-based approach to achieving interoperability in the healthcare domain. Unlike HL7, FHIR is modular, allowing you to tailor data exchange to your needs. Choose the resources you need, like medications, allergies, or diagnoses, and leave the rest behind. FHIR also plays well with others. It readily integrates with existing HL7 standards and other systems, bridging the gap between different technologies.
While the ONC (Office of the National Coordinator for Health Information Technology) doesn’t explicitly mandate using FHIR across all healthcare contexts, several important ONC rules heavily incentivize and promote its adoption.
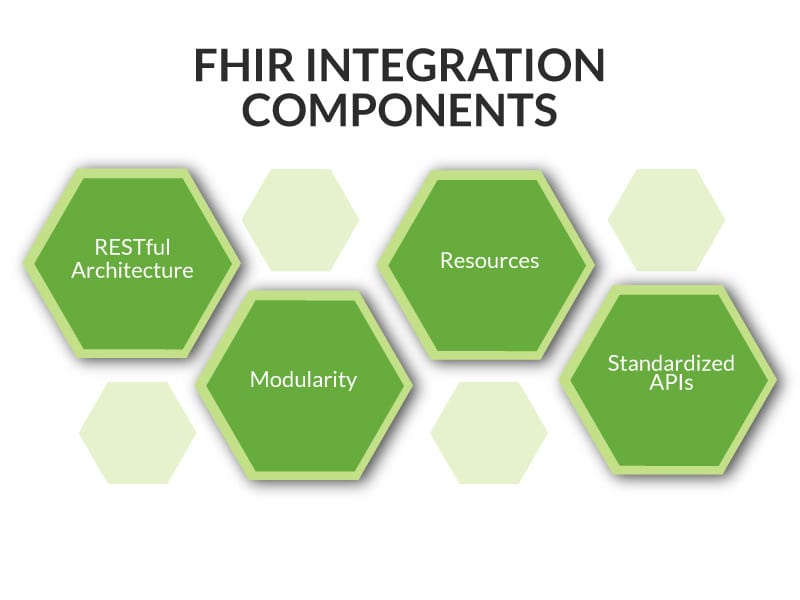
Key components and benefits of FHIR:
-
- RESTful Architecture: FHIR adopts a RESTful (Representational State Transfer) approach, utilizing standard web protocols. This design choice enhances flexibility and simplifies data exchange between healthcare systems.
- Modularity: FHIR’s modular design allows for incremental adoption, enabling healthcare organizations to implement specific resources or components without undertaking a complete system overhaul. This flexibility supports a phased approach to interoperability.
- Resources: FHIR introduces the concept of “resources” as the fundamental building blocks. These resources represent discrete clinical or administrative information, such as patients, medications, and observations.
- Standardized APIs: FHIR leverages standardized APIs (Application Programming Interfaces) to facilitate seamless communication between healthcare applications. These APIs ensure efficient data exchange and enable developers to create interoperable solutions.

Challenges of FHIR
FHIR holds immense promise and has introduced significant improvements in healthcare data exchange. However, it’s important to acknowledge that it’s still evolving and does have some challenges and limitations.
- Implementation Complexity: FHIR’s flexibility and modularity, while beneficial, can also lead to implementation complexity. Healthcare organizations and developers may find navigating and implementing specific aspects of the FHIR standard challenging.
- Variability in Adoption: FHIR adoption varies among healthcare organizations, and the transition from older standards like HL7 v2 to FHIR may be slow. Existing health IT systems may not readily support FHIR, leading to a fragmented interoperability landscape.
- Data Consistency: FHIR’s flexibility allows for the creation of custom profiles and extensions. While this adaptability is advantageous, it can result in data representation and consistency variations, affecting interoperability.
- Semantic Interoperability Challenges: Achieving true semantic interoperability, where data is structurally and semantically aligned, remains a challenge. Differences in terminology and coding systems across healthcare systems can hinder seamless data exchange.
- Resource Versioning: Managing different versions of FHIR resources can be complex. As FHIR evolves, updates may occur, and healthcare organizations must handle versioning to ensure compatibility and consistency in data exchange.
- Interoperability with Legacy Systems: Healthcare organizations often have legacy systems that may not easily integrate with FHIR. Bridging the gap between modern FHIR-based systems and older technologies poses challenges in achieving comprehensive interoperability.
- Global Standardization: While FHIR has gained international recognition, regional variations in implementation and compliance may exist. Achieving global standardization and uniformity in FHIR adoption can be a gradual process.
Despite these challenges, FHIR represents a significant step forward in healthcare interoperability. Ongoing efforts within the FHIR community, collaboration with healthcare stakeholders, and advancements in supporting technologies aim to address these limitations and enhance the overall effectiveness of FHIR in healthcare data exchange. FHIR is constantly improving, paving the way for a future where healthcare data flows freely, empowering better care for everyone.
Interoperability Standards: the Linchpin of Healthcare Technology
In conclusion, interoperability standards, particularly FHIR, are a critical linchpin in the evolution of healthcare technology. As we’ve delved into the importance of seamless data exchange, it’s evident that interoperability standards are a foundation for a connected healthcare ecosystem. However, it’s crucial to recognize that while FHIR has emerged as a promising standard, it’s not a one-size-fits-all solution. Achieving true interoperability requires a strategic blend of diverse approaches, acknowledging the complex web of technologies, workflows, and methodologies contributing to a robust, data-driven healthcare landscape.
As we continue our journey toward a more interconnected healthcare system, our next blog post, “EHR Interoperability: Exploring the Pros and Cons of Different Approaches,” will guide you through the varied methods that, when combined effectively, propel us closer to achieving the seamless data exchange envisioned for the future of healthcare. Join us in uncovering the intricacies of EHR integration as we navigate the diverse routes that collectively lead to a more connected and efficient healthcare ecosystem.
Naveen Vangipurapu, VP Software Development
Table of Contents




