Value-Based Care: The Ultimate Guide
What is Value-Base Care?
Simply put, value-based care is a shift in the reimbursement model between healthcare insurers and providers. Instead of being paid per service delivered, providers receive incentives based on the results they deliver, emphasizing the quality, equity, and cost-effectiveness of care. By employing financial incentives and other methods such as shared financial risk, value-based programs aim to hold providers accountable for enhancing patient outcomes while allowing them more flexibility to provide timely, appropriate care.
Why is Value-Based Care Needed in Healthcare?
The answer to this question is surprisingly simple. The healthcare system is out of control when it comes to spending. In fact, the Medicare Trust Fund is expected to be depleted by approximately 2031. For decades, the Fee-For-Service (FFS) model has been the predominant payment structure. It emerged from the need to compensate healthcare providers for their work, ensuring they were paid for every service provided. Initially, this model seemed logical and fair, aligning payment directly with the type of care service delivered. Over time, the flaws in this arrangement have become cripplingly clear.
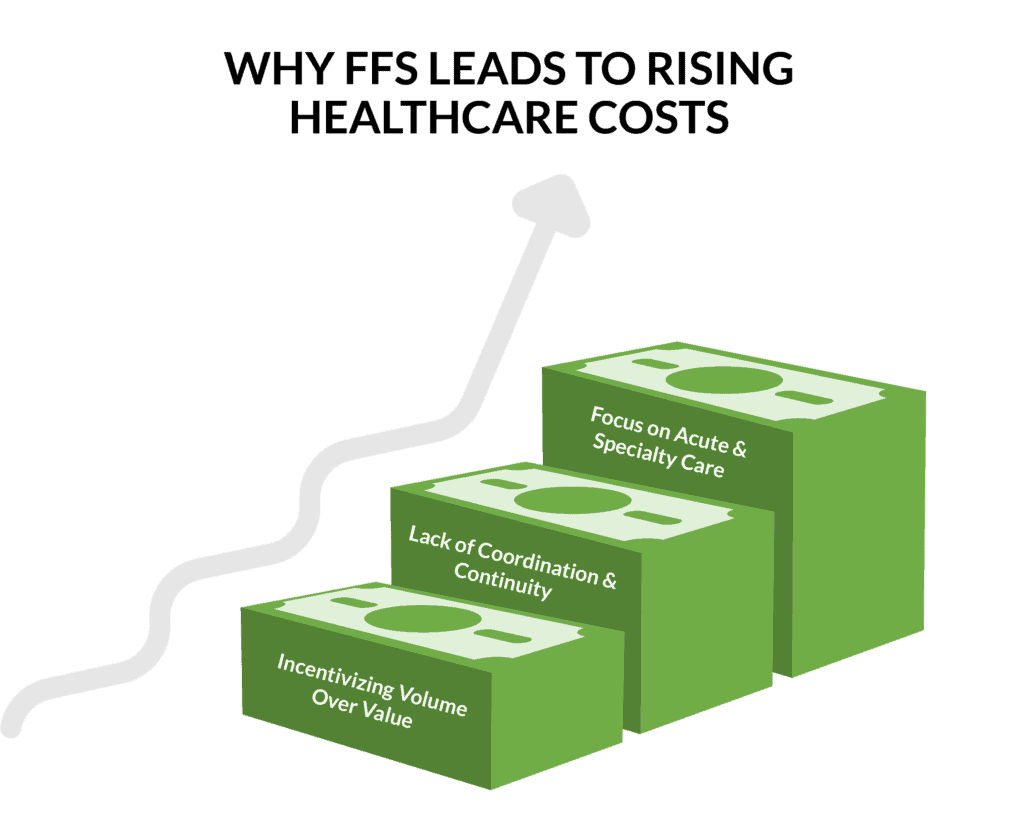
Why FFS Leads to Rising Healthcare Costs:
- Incentivizing Volume or Value: When providers are financially rewarded for delivering more services, regardless of whether those services are necessary or contribute to better patient outcomes, overutilization of services naturally occurs. Things like duplicate diagnostic testing, procedures, follow-up visits, and hospitalizations all add up, skyrocketing the overall cost of care.
- Lack of Coordination and Continuity: Under FFS, there is little financial incentive for providers to coordinate with one another. This has resulted in fragmented care, with multiple providers ordering duplicate tests or procedures, or patients receiving inconsistent care plans. Poor coordination has led to inefficiencies, increased costs, and patient dissatisfaction and faith in the system.
- Focus on Acute and Specialty Care: FFS tends to favor acute and specialty care over preventive care and chronic disease management. Providers are paid more for treating existing conditions and performing surgeries and specialized procedures than for managing chronic conditions or offering preventive services. This imbalance results in higher costs due to the emphasis on treatment rather than prevention.
The FFS model is often referred to as ‘reactive’ care. Its primary focus is on providing and billing for individual healthcare services after patients become ill. This means that care often comes too late to prevent disease progression or complications. Preventive measures, such as vaccinations, screenings, and lifestyle counseling, are not prioritized under FFS because they typically generate lower immediate revenue compared to acute care interventions. As a result, opportunities to prevent diseases and detect conditions early are often missed.
Value-based care, a more proactive approach, began gaining traction in the early 2000s. Its origins are rooted in the fundamental premise that preventing diseases is generally much cheaper than treating them after they develop. For example, diabetes, which is one of the highest expenditures for Medicare, is preventable simply by screening people for metabolic disorder and putting them on a personalized preventive plan.
Key Legislative Milestones in the Transition to Value Based Care
The overarching goal of value-based care is to enhance patient outcomes while controlling healthcare costs, ultimately leading to a more sustainable healthcare system. Patient outcomes refer to the measurable changes in health, quality of life, and satisfaction that result from healthcare services and interventions. These outcomes are critical indicators of the effectiveness, quality, and efficiency of healthcare delivery. They help evaluate how well healthcare systems and providers are achieving their primary goal: improving the health and well-being of patients.
The shift to value-based care has been marked by several key milestones and significant legislation to improve healthcare quality, patient outcomes, and cost efficiency. Here are some of the most notable developments:
- 1983: Introduction of Prospective Payment System (PPS)
- The PPS was implemented for Medicare hospital payments, replacing the cost-based reimbursement system. This system introduced fixed payment amounts for patient diagnoses, incentivizing hospitals to control costs and improve efficiency.
- 2001: Institute of Medicine (IOM) Report
- The IOM (now the National Academy of Medicine) published a game-changing report called “Crossing the Quality Chasm: A New Health System for the 21st Century.” This report highlighted the need for a healthcare system emphasizing quality, safety, and efficiency and laid the groundwork for value-based care principles.
- 2006: Introduction of Pay-for-Performance (P4P) Programs
- Medicare began pilot programs that rewarded healthcare providers for meeting specific quality benchmarks. These programs aimed to align financial incentives with quality improvements and better patient outcomes.
- 2008: Medicare Improvements for Patients and Providers Act (MIPPA)
- MIPPA expanded Medicare’s Quality Improvement Organization (QIO) program and introduced incentives for healthcare providers to use electronic health records (EHRs), promoting better care coordination and patient management.
- 2009: Health Information Technology for Economic and Clinical Health (HITECH) Act
- Part of the American Recovery and Reinvestment Act (ARRA), the HITECH Act provided financial incentives for healthcare providers to adopt and meaningfully use EHRs. This act aimed to improve care quality, safety, and efficiency through better information sharing.

- 2010: Patient Protection and Affordable Care Act (ACA)
- The ACA was a significant legislative milestone that accelerated the shift to value-based care. Key provisions included:
- Accountable Care Organizations (ACOs): Encouraged the formation of ACOs, groups of providers who collaborate to improve care quality and reduce costs for a defined patient population.
- Hospital Readmissions Reduction Program (HRRP): Penalized hospitals with high readmission rates for certain conditions, incentivizing better discharge planning and follow-up care.
- Value-Based Purchasing (VBP) Program: Linked hospital payments to performance on quality measures, rewarding high-performing hospitals and penalizing low performers.
- Medicare Shared Savings Program (MSSP): Allowed ACOs to share in savings they generated for Medicare by improving care and reducing costs.
- The ACA was a significant legislative milestone that accelerated the shift to value-based care. Key provisions included:
- 2015: Medicare Access and CHIP Reauthorization Act (MACRA)
- MACRA introduced the Quality Payment Program (QPP), which replaced the Sustainable Growth Rate (SGR) formula. The QPP includes two tracks:
- Merit-based Incentive Payment System (MIPS): Adjusts payments based on performance in quality, cost, improvement activities, and the use of EHRs.
- Advanced Alternative Payment Models (APMs): Provides incentives for providers to participate in innovative payment models that emphasize high-quality, cost-efficient care.
- MACRA introduced the Quality Payment Program (QPP), which replaced the Sustainable Growth Rate (SGR) formula. The QPP includes two tracks:
- 2016: Comprehensive Primary Care Plus (CPC+) Initiative
- CPC+ is a primary care medical home model that offers financial incentives and support to primary care practices to improve care coordination, access, and quality.
- 2020: Advancing American Kidney Health Initiative
- This initiative aimed to transform kidney care by encouraging preventive care, home dialysis, and kidney transplants. It included new payment models to support these goals.
- 2021: Center for Medicare and Medicaid Innovation (CMMI) Strategic Refresh
- CMMI announced a strategic refresh to focus on five key objectives: driving accountable care, advancing health equity, supporting innovation, addressing affordability, and partnering to achieve system transformation.
- Ongoing: State-Level Innovations and Private Sector Initiatives
- Various states and private payers have also implemented value-based care models, such as Medicaid managed care programs and private insurer value-based contracts, to improve care quality and reduce costs.
It’s important to note that the healthcare landscape is dynamic, and new legislative initiatives may have emerged or are in progress. So far, the shift as a whole hasn’t been an easy one. Many providers struggle because they lack the technologies needed to access data and efficiently track and report on their performance measures. Yet, the Centers for Medicare and Medicaid Services (CMS) has set a goal of enrolling all Medicare beneficiaries and most Medicaid beneficiaries in accountable care programs by 2030. Historically, commercial payers follow CMS’s lead.
What are the Key Benefits of Value-Based Care?
Value-based care (VBC) offers numerous benefits for patients, healthcare providers, and the healthcare system as a whole. Below is a high-level list of the key benefits:
- Improved Patient Outcomes
- Better Quality of Care: Evidence-based practices, leading to higher quality care and better clinical outcomes.
- Focus on Prevention: Preventive measures and early interventions reduce the incidence and severity of diseases, improving overall health.
2. Enhanced Patient Experience
- Patient-Centered Care: Care is tailored to individual patient needs, preferences, and values, enhancing patient satisfaction.
- Improved Coordination: Integrated care and better
communication among providers leads to a smoother and more cohesive care experience.
3. Cost Savings
- Reduced Waste: By eliminating unnecessary tests and procedures, VBC reduces wasteful spending.
- Lower Healthcare Costs: Preventive care and effective management of chronic conditions lower the need for expensive emergency and inpatient care.
4. Increased Efficiency
- Streamlined Processes: Coordinated care and the use of health information technology streamline administrative processes and reduce redundancies.
- Resource Optimization: Efficient use of resources ensures that healthcare spending is directed towards effective treatments and interventions.
5. Financial Incentives
- Performance Based Payments: Providers are rewarded for achieving positive health outcomes and cost savings, aligning financial incentives with quality care.
- Risk Sharing: Payment models that include shared savings and risk encourage providers to deliver cost-effective, high-quality care..
6. Promotion of Health Equity
- Addressing Disparities: VBC initiatives often include measures to reduce health disparities and improve access to care for underserved populations.
- Incentives for Equity: Providers may receive financial incentives to ensure equitable care delivery and reduce health disparities.
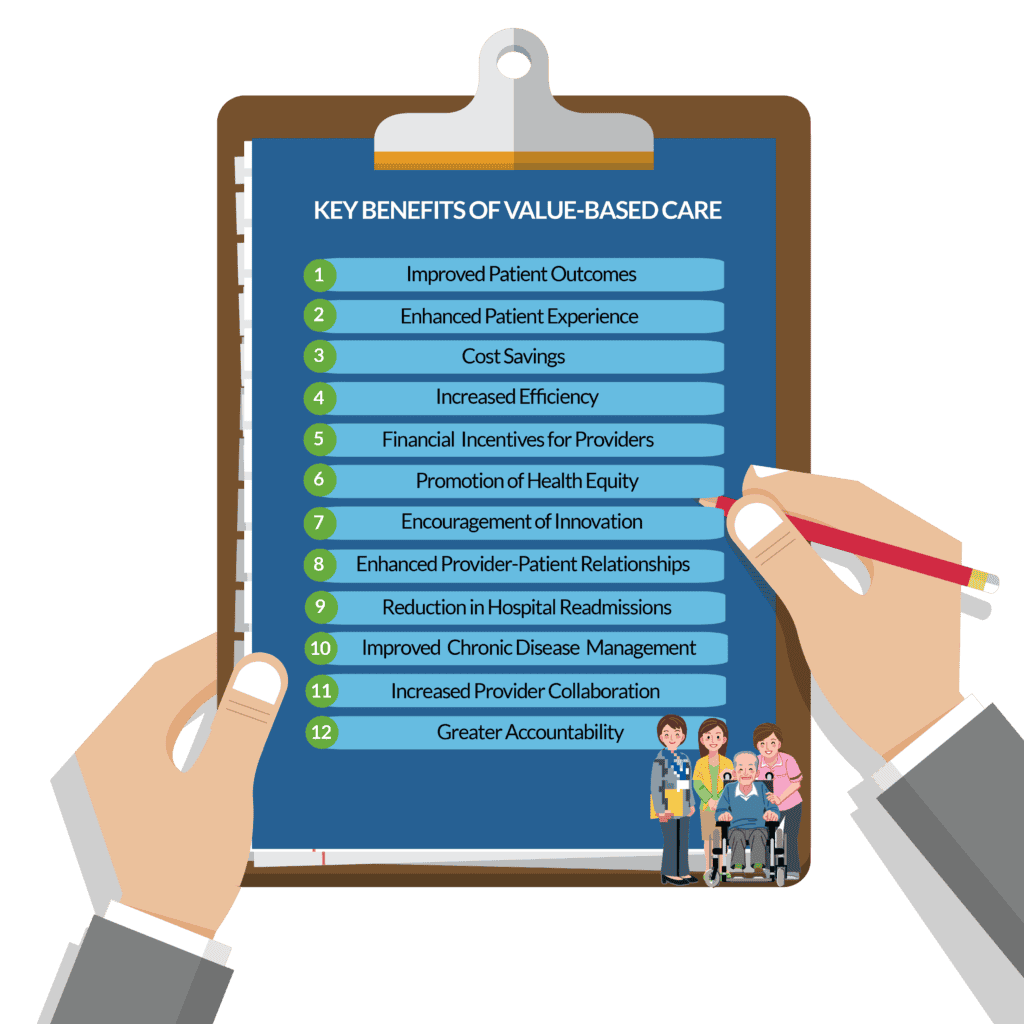
7. Encouragement of Innovation
- New Care Models: VBC promotes the development of innovative care models, such as Accountable Care Organizations (ACOs) and Patient-Centered Medical Homes (PCMHs), which enhance care quality and efficiency.
- Health IT Adoption: The use of electronic health records (EHRs) and telemedicine supports better care coordination and patient monitoring.
8. Enhanced Provider-Patient Relationships
- Engaged Patients: Educating and involving patients in their care leads to better adherence to treatment plans and improved health behaviors.
- Trust and Communication: Stronger relationships between patients and providers result in better communication, trust, and overall care satisfaction.
9. Reduction in Hospital Readmissions
- Effective Post Acute Care: Better discharge planning and follow-up care reduce the likelihood of hospital readmissions, which are costly and often indicative of poor care quality.
10. Improved Chronic Disease Management
- Proactive Management: Regular monitoring and management of chronic conditions prevent complications and hospitalizations, improving patients’ quality of life.
11. Increased Provider Collaboration
- Team Based Care: Collaborative care models encourage multidisciplinary teams to work together, enhancing care quality and patient outcomes.
12. Greater Accountability
- Performance Measurement: Regular evaluation of provider performance ensures accountability and continuous improvement in care delivery.
How to Implement Value-Based Care
Implementing value-based care within a provider organization requires strategic planning, stakeholder engagement, and the adoption of new processes and technologies. Best practices for a successful implementation involves a three-phase approach that provides a structured pathway for healthcare organizations to transition successfully. By starting with a thorough assessment, setting clear and measurable goals, and executing well-negotiated contracts with the right partners, organizations can achieve the promise of value-based care. This approach not only enhances care coordination, patient outcomes, and cost management but also positions the organization for long-term success in an increasingly value-driven healthcare environment. With committed leadership and a focus on continuous improvement, healthcare organizations can lead the way in revolutionizing care delivery in the United States.
Many organizations hire a value-based consultant to oversee the project and provide input along the way. These consultants bring deep industry knowledge, proven strategies, and experience in navigating the complexities of value-based models, ensuring a smoother transition from fee-for-service structures. They help identify and address gaps in care delivery, financial structures, and operational workflows, while also offering guidance on selecting the right value-based contracts and technology solutions. By leveraging their expertise, your organization can more effectively improve patient outcomes, reduce costs, and achieve long-term financial sustainability in the competitive healthcare landscape.
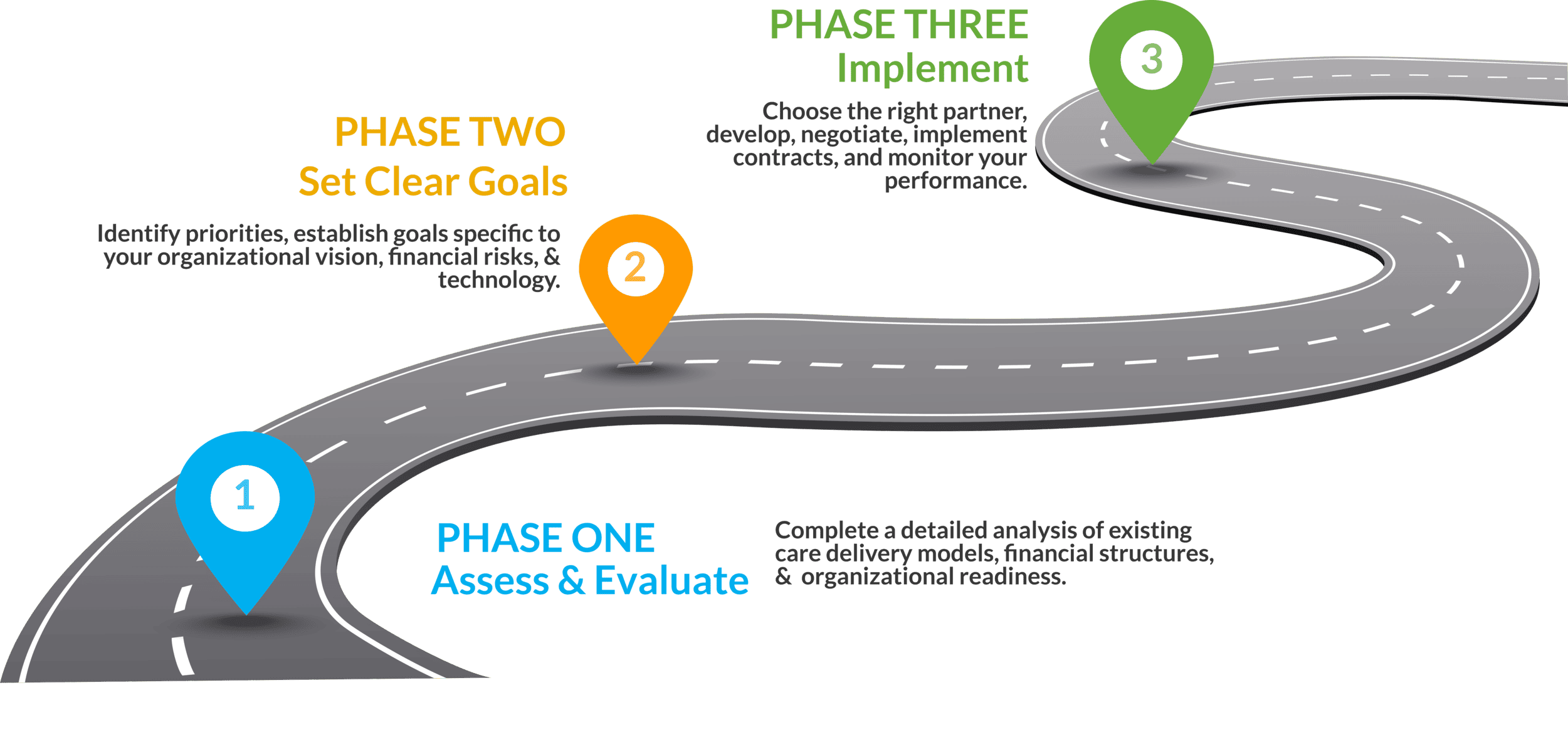
PHASE ONE: ASSESS AND EVALUATE
This is the initial phase and includes completing a detailed analysis of existing care delivery models, financial structures, and organizational readiness for change.
PHASE TWO: SET CLEAR GOALS
In this phase, you gather the data from Phase One, do a deep dive on priorities, and establish goals specific to your organizational vision, financial incentives and risk management. You’ll consider the technology you’ll need to leverage, and best practices for staff engagement.
PHASE THREE: IMPLEMENT
Phase Three is where the rubber meets the road. In this phase, you’ll educate yourself on the types of value-based contracts, choose the right partner for your organization, develop, negotiate, and implement contracts, and monitor your performance.
Common Value-Based Care Challenges and Solutions
Making the transition to value-based payment models is not easy and takes time. Below are some of the common challenges you will face on this journey and some potential solutions:
1. Financial Risk and Stability
CHALLENGE: Increased financial risk due to the unpredictability of shared savings and the potential for losses.
SOLUTIONS:
- Gradual Transition: Implement a phased approach to transition, starting with upside-only risk models where providers share savings without risking losses.
- Risk Adjustment: Use risk adjustment methodologies to account for patient population differences and reduce financial unpredictability.
- Stop-Loss Insurance: Purchase stop-loss insurance to protect against significant financial losses.
2. Data Management and Analytics
CHALLENGE: Value-based care requires robust data analytics to track patient outcomes, costs, and performance metrics. Many providers struggle with integrating and analyzing data from disparate sources.
SOLUTIONS:
- Invest in Technology: Invest in advanced electronic health record (EHR) systems and data analytics platforms to facilitate data integration and analysis.
- Partnerships: Partner with technology vendors or data analytics firms that specialize in healthcare data management. One of the most important aspects of provider adoption is to ensure the information needed for value-based metrics such as, diagnosis confirmation and/or gap closure can be done within the EHR system. Ensure the technology partner you choose can provide the necessary data in the EHR.
3. Care Coordination
CHALLENGE: Coordinating care across multiple providers and settings is essential for value-based care but can be complex and resource-intensive.
SOLUTIONS:
- Care Management Programs: Develop comprehensive care management programs to support care coordination, including hiring care coordinators or case managers directly or contracting with a care management services company.
- Integrated Care Pathways: Create integrated care pathways that standardize care processes for your most expensive disease states across your providers.
- Communication Tools: Leverage communication tools such as secure messaging platforms, referral management solutions, and shared care plans to enhance coordination among care teams.
4. Patient Engagement
CHALLENGE: Effective patient engagement is crucial for value-based care but can be difficult to achieve, especially with populations that have low health literacy or limited access to healthcare resources.
SOLUTIONS:
- Patient Education: Develop patient education programs to inform patients about their health conditions, treatment options, and the importance of preventive care.
- Digital Tools: Use digital tools such as patient portals, mobile health apps, and telemedicine to engage patients in their care and provide easy access to health information.
- Community Outreach: Conduct community outreach programs to engage underserved populations and address social determinants of health.
5. Measuring and Reporting Outcomes
CHALLENGE: Measuring and reporting outcomes accurately is critical for value-based care but can be challenging due to the complexity of defining and tracking appropriate metrics.
SOLUTIONS:
- Clear Metrics: Define clear, measurable metrics for evaluating performance and outcomes, aligned with value-based care goals.
- Benchmarking: Use benchmarking tools to compare performance against industry standards and identify areas for improvement.
- Continuous Monitoring: Implement continuous monitoring systems to track progress and adjust strategies as needed based on real-time data.
What Success has Value Based Care Achieved?
To date, much of the value-based care successes have been in specific areas, particularly in acute and specialty care. For instance, in focused populations like end-stage kidney disease and oncology, organizations have effectively utilized targeted analytics and care coordination to address avoidable expenses comprehensively.
VBC models aim to slow or reduce the overall growth of healthcare costs while simultaneously improving the quality of care. For VBC to achieve a more significant impact on a larger scale, the industry needs to prioritize coordinated, evidence-based medicine and proactive care across the continuum. These are not just strategies but essential components for the success of VBC.
What’s Next in Value-Based Care?
Key healthcare advisory firms are anticipating that value-based care will accelerate. Per Brian Fuller, Managing Director of ATI Advisory’s Value-Based Care Design and Delivery practice, many organizations are either revisiting their VBC strategies or implementing them for the first time. With 13 million Medicare beneficiaries under ACO or VBC arrangements in 2023, and the CMS Innovation Center’s goal to have all Medicare beneficiaries in an accountable relationship by 2030, the demand for VBC will rise. This growth is driven by fiscal and demographic trends, new VBC models from CMMI, and Medicare’s expanding enrollment.

Investment in Primary Care
Fuller emphasized that successful value-based care hinges on improving primary care in three key areas: access, capacity, and capabilities. Many regions in the U.S., including 77% of rural counties, are considered primary care deserts. Despite shorter appointment wait times since 2017, more primary care physicians are opting out of Medicare and Medicaid. Additionally, most primary care practices lack VBC capabilities such as site-neutral delivery, which are crucial for participating in VBC models effectively.
Emergent and Legacy Players
Traditional healthcare providers, such as primary care physicians, hospital systems, and ACOs, cannot fully meet the comprehensive needs of the increasing number of VBC beneficiaries. This creates opportunities for new players like community pharmacies and home care providers to fill gaps left by legacy providers. These emergent players can form trusted relationships through frequent interactions and community engagement, improving transitional care and closing quality care gaps.

The Role of Specialty Care
Outpatient care for Medicare beneficiaries has increasingly shifted towards specialty visits since 2009, with no corresponding shift in primary care visits. This trend presents an opportunity to integrate specialty care more effectively into VBC models. CMS has released RFIs to explore these opportunities, and private equity investment in specialty care areas such as dementia and chronic kidney disease has grown.
Innovation Through Medicare Advantage
Medicare Advantage (MA) offers more flexibility and design incentives than traditional fee-for-service Medicare. Fuller highlighted several factors expected to drive innovation in MA plans in 2024, including the blurring of lines between payer and provider, increased financial pressures due to the RADV rule, and the removal of FFS adjusters.
Additional Trends to Watch
- Episode-of-care and bundled payments: Driving focus and flexibility across VBC payment structures.
- Post-hospital throughput challenges: Intersecting with VBC efforts.
- Medicaid innovation: Emerging as a new frontier in VBC, especially for complex and vulnerable populations.
- Health equity and SDOH integration: Requiring new clinical, operational, and financial constructs.
Fuller concluded by emphasizing the importance of having a well-defined and refreshed value-based care strategy to navigate current market dynamics and seize emerging opportunities.
Table of Contents
If your team is ready for a solution that can support your value-based care initiatives, let's talk.
Contact us today at 877-502-3067 or info@smartlinkhealth.com.


